Struggling with Postpartum Mood Disorder? New medication can help!
The FDA just approved the first-ever medication that was designed specifically to treat postpartum depression with fast results. Although there is a long way to go in the battle to fully support all Moms, this great milestone is a great milestone for progress with postpartum mood disorders.
In this blog we'll delve into relevant statistics, offering insight into the prevalence of Postpartum Mood Disorders and its correlation with sleep deprivation, backed by credible references.
New Postpartum Medication
Here are some highlights of this new postpartum medication, Zurzuvae (zuranolone):
Oral pill that can swiftly improve depressive symptoms
Taken once a day for two weeks
Resets brain functions related to mood, arousal, behavior and cognition, and helps the brain cope with stress again.
Expected to release late 2023
Read more in the Huffington Post article.
Baby Blues vs Postpartum Mood Disorders
Baby blues, also known as postpartum blues, are common and transient mood changes that many new mothers experience shortly after giving birth. Baby Blues affects up to 80% of new mothers and is considered a normal response to the significant hormonal and emotional adjustments that occur during the postpartum period. It's important to note that baby blues typically occur within the first few days after childbirth and may last up to two weeks. Postpartum Mood Disorders cover the following: depression, anxiety, OCD and other mood disorders start to persist and can be relentless and get worse and last long.
Postpartum Mood Disorders cover the following:
Postpartum Depression (PPD): The most common postpartum mood disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in daily activities.
Postpartum Anxiety Disorders: A group of anxiety disorders that may occur postpartum, including generalized anxiety disorder, panic disorder, and postpartum obsessive-compulsive disorder (OCD).
Postpartum Obsessive-Compulsive Disorder (OCD): A subtype of anxiety disorder characterized by distressing, intrusive thoughts and repetitive behaviors or rituals related to the baby's safety or well-being.
Postpartum Panic Disorder: An anxiety disorder marked by recurrent, unexpected panic attacks, which can involve intense fear and physical symptoms like a rapid heartbeat and shortness of breath.
Postpartum Post-Traumatic Stress Disorder (PTSD): Occurs when a woman experiences distressing or traumatic events during childbirth, leading to symptoms like flashbacks, nightmares, and severe anxiety.
Postpartum Bipolar Disorder: A condition where a woman experiences episodes of depression and mania (elevated mood, impulsivity) in the postpartum period, which can disrupt her ability to function.
Postpartum Psychosis: A rare but severe condition marked by hallucinations, delusions, disorganized thinking, and rapid mood swings, often requiring immediate medical intervention.
Postpartum Adjustment Disorder: A milder form of emotional distress that may include symptoms like irritability, mood swings, and difficulty coping with the challenges of new motherhood.
How Common is Postpartum Mood Disorders
Postpartum Mood Disorders affects around 10-20% of women (American Psychological Association, APA).
Postpartum Depression how long does it last
Postpartum Mood Disorders is a form of clinical depression and anxiety that occurs after childbirth.
Onset of symptoms: PPD typically starts within the first few weeks to months after giving birth. However, for some individuals, it can begin during pregnancy or appear later in the postpartum period up to 3 years after birth.
Duration of symptoms: It's essential for women experiencing PPD to seek help and support from healthcare professionals, therapists, and support groups. Early intervention and appropriate treatment can significantly improve outcomes and help shorten the duration of PPD. It's important to remember that PPD is a treatable condition, and with the right support, most women can recover and return to their normal functioning and well-being.
The Link Between Sleep and Postpartum Mood Disorders
Sleep deprivation is a common issue for new mothers, especially during the early months of their baby's life. The demanding schedule of caring for an infant can lead to disrupted sleep patterns and, in some cases, severe sleep deprivation. Emerging research has shown a clear connection between sleep and postpartum mood disorders.
Sleep Deprivation and Hormonal Changes: During sleep, the body undergoes critical hormonal processes, including the regulation of serotonin and cortisol levels. Disrupted sleep can interfere with these processes, impacting mood regulation and leading to depressive symptoms.
Circadian Rhythm Disruptions: The postpartum period can significantly disrupt a woman's circadian rhythm, the internal clock that regulates sleep-wake cycles. This disruption further exacerbates sleep problems and can contribute to the development of postpartum mood disorders.
Bidirectional Relationship: The relationship between sleep and postpartum depression is bidirectional. While sleep deprivation can contribute to PPD, the presence of depression, anxiety, OCD, etc can also lead to sleep disturbances, creating a vicious cycle that affects a new mother's mental health.
Postpartum Mood Disorders is a serious and prevalent condition that can affect new mothers regardless of cultural or socioeconomic backgrounds. Understanding the significance of sleep in the development of PPD is crucial for early detection and intervention. As society becomes more aware of the challenges faced by new mothers, it is essential to offer comprehensive support systems that encompass mental health care, sleep support, and understanding.
If you or someone you know is experiencing postpartum depression symptoms, do not hesitate to seek professional help. Early diagnosis and appropriate treatment can significantly improve a mother's well-being and positively impact her baby's development. Together, we can foster a supportive environment for new mothers and contribute to a healthier and happier postpartum experience.
The key take away, if you are not feeling "like yourself", please don't hesitate to ask for help. Here are some resources.
Blue Dot Maternal Health Resources and Overview of Mood Disorders
https://www.thebluedotproject.org/whataremmhdisorders
Postpartum National Support Hotline
https://www.2020mom.org/get-help
GREAT BOOK!!
Good Moms Have Scary Thoughts: Karen Kleiman
Over 90 percent of new mothers will have scary, intrusive thoughts about their baby and themselves. What if I drop him? What if I snap and hurt my baby? Mothering is so hard. I don't know if I really want to do this anymore. Gosh, I'm so terrible for thinking that! Yet for too many mothers, those thoughts remain secret, hidden away in shame that make you feel even worse. But here's the good news: you CAN feel better!
Author Karen Kleiman, coauthor of the seminal book This Isn't What I Expected and founder of the acclaimed Postpartum Stress Center, comes to the aid of new mothers everywhere with a groundbreaking new source of hope, compassion, and expert help. Good Mothers Have Scary Thoughts is packed with world-class guidance, simple exercises, and nearly 50 stigma-busting cartoons from the viral #speakthesecret campaign that help new moms validate their feelings, share their fears, and start feeling better. Lighthearted yet serious, warm yet not sugary, and perfectly portioned for busy moms with full plates, Good Moms Have Scary Thoughts is the go-to resource for moms, partners, and families everywhere who need help with this difficult period..
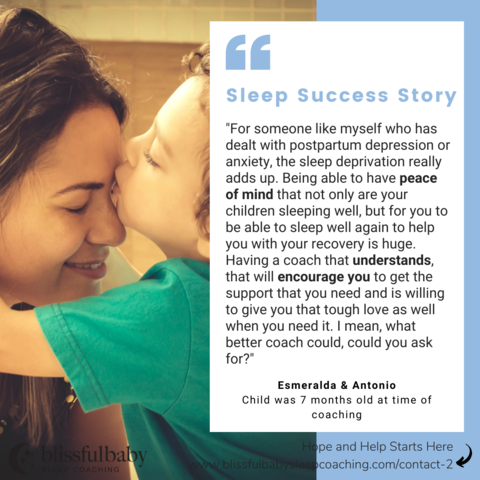
Success Stories
Clients have found Sleep Coaching their child has had an incredible impact on supporting Mom and their postpartum depression. Teaching your child the skills of sleep has benefits beyond "just sleep."
Mom had dealt with postpartum depression and anxiety was able support her own recovery while also having the the confidence and peace her children were sleeping well.
Mom felt she was unraveling mentally, physically, and emotionally after the birth of her daughter when her pediatrician referred her to Blissful Baby Sleep Coaching for support.
"Postpartum depression was one of the biggest challenges and I didn't see it coming. I was in that kind of a fog phase of just giving birth the hormones, the whole newness of it all, a newborn and then not sleeping. That's just a recipe for disaster and the depression, it just came on. It was pretty quick. After getting help and sleep coaching, I was able to get sleep and kind of rest. I woke up and I remember feeling like a new person, a completely new woman just because I got some sleep."
As a Pediatric Sleep Consultant, I work closely with sleep-deprived families and many of the Mom have also struggled with Postpartum Mood Disorders. As part of my Gentle Sleep Process, I assess families unique situation, history and goals when co-creating an individualized sleep plan. I want all families to feel supported, with "a village." The end result of my sleep coaching services is feeling good about sleep training AND a great night’s sleep for everyone because getting great sleep for your child creates the momentum and focus you need to feel more like yourself.
Are you struggling with your child's sleep?
The first step to see if I can help you achieve beautiful, blissful sleep is to schedule a 60 minute ZOOM sleep strategy session. Go to this link and complete the contact me form and I will be in touch within 24 hours with directions on how to schedule your Sleep Strategy Session.
If you are still wondering if I can help, please know I do NOT advocate 'cry-it-out'. I am a Gentle Sleep Coach. If you want to learn about my guilt-free and gentle process, please go to these links.
The Blissful Baby Stairway to Sleep
Please join my Sleep is Bliss Tribe in Facebook, Instagram and LinkedIn so we can stay connected and you can continue to get amazing resources on sleep and family wellness.